Research roundup 2023
Here are my favourite papers of the year
Every day in December I’ve been posting the best papers I’ve come across this year. It has been a bit of fun but also a chance to reflect on how science is progressing. Looking back at my list, some themes emerge.
We’re in a new era of neuroimaging. There are many more papers with large enough sample sizes to make findings believable. Last year’s demonstration that thousands of participants are required for brain wide association studies clearly hit home.
Big data is bearing fruit. Amazing resources like the UK Biobank, or record linkage of health records is continuing to provide researchers with the sample sizes needed to ask complex questions about health.
Optogenetics is an incredible tool. The precise neuronal circuitry is being described for various biological processes. When will the Nobel prize for this methodological leap forward arrive?
Hormonal mechanisms are being discovered. From oxytocin, to GDF15, neuroendocrinology is booming. With the approval of neurokinin-3 receptor antagonists following a number of novel hormone-based medications (zuranolone, semaglutide, daridorexant). I can only see the field growing.
The RCT is still king. When an answer is needed in medical science, a well conducted randomised trial continues to reign supreme.
Below is a summary of my favourite papers. Are any of them duds? What did I miss? Was I dazzled by the glamour journals?
Please tell me in the comments. And have a happy Christmas everyone!
Countdown
This study included 5k people with schizophrenia and 6k unaffected controls, gathered from 46 separate datasets. The authors report 7% of the variance in brain asymmetry was linked to case-control status. Specifically, they found a reduction of the usual left-asymmetry in the middle temporal region.
Why should you care? Human brains are naturally asymmetrical - most people are right-handed, meaning their left hemisphere is dominant. But with schizophrenia, more people are left handed than expected. I’ve previously discussed why this increase in left-handedness and differences in usual brain asymmetry could be explained by shared neurodevelopmental factors that later lead to the development of schizophrenia.
Homeopathy is a perfect ‘null field’. There is no plausible mechanism for it to work. Despite this, there is a wealth of published research, much of it in reputable journals. In effect, the field of homeopathy can act as a control to compare with other scientific fields.
This paper takes a sample of 50 randomised placebo-controlled trials of homeopathy and extracts features. Overall, they calculate an effect size (Hedge’s g) of 0.36 versus placebo - does this look familiar? Yes, it’s the same size as antidepressants over placebo!
To be clear, I do not think antidepressants are equivalent to homeopathy, however, it does show how far researcher bias can push an inactive treatment (homeopathy) over another inactive treatment (placebo).
You know I love the neurokinin-3 receptor antagonist story - a failed medication for schizophrenia being repurposed for menopausal symptoms. SKYLIGHT 1 was one of the trials that led to its FDA and MHRA approval this year.
The trial, as expected from a pharma company has a large sample size (n=175 per arm), transparent reporting, and pre-defined outcomes. The drug had clear, sustained benefits over placebo and was well tolerated.
Clinical recovery and long-term association of specialised early intervention services vs treatment as usual among individuals with first-episode schizophrenia spectrum disorder: 20-year follow-up of the OPUS trial
The UK, like many countries, has restructured mental health service to provide early intervention in psychosis. The logic is to intervene before psychotic disorders take root. It makes sense that directing our focus at the earliest stages of illness would provide long-term benefits.
This study by Hansen and colleagues looked at the 20 year follow-up data from a randomised controlled trial of early intervention in psychosis versus treatment as usual (n=547).
Attrition was substantial (only 30% of the participants could be interviewed). However, the wonderful Danish record-linkage system allowed the authors to compare the health records of all participants. There was no benefit from early intervention on outcomes such as mortality, psychiatric admission, or employment, calling into question the long-term benefits of this approach.
This is the first (but not last) paper on my list to investigate connections between the heart and brain. The authors took advantage of the UK Biobank to examine individuals who had both brain and cardiac MRI scans. The sample size >30k gives incredible power to investigate the connections between these two organs.
There were many associations between volumes of brain structures and heart structures (with a study this big, we would expect to identify associations, even if the signal is weak). They also used genetic data to identify shared contribution to cardiac and brain imaging.
We already know that natural reproductive events like childbirth, the menstrual cycle, and menopause can trigger depressive episodes. We also know that there is some connection between these events - women who have a history of premenstrual dysphoric disorder are more at risk of postpartum depression.
How does hormonal contraception fit into this? If there is a subgroup who are vulnerable to the effects of endogenous and exogenous hormones, we would expect episodes of depression triggered by hormonal contraception to be a risk factor for postpartum depression.
Larsen and colleagues found that those with depression associated with hormonal contraception had 1.4 times the rate of postpartum depression compared to those who had depression not associated with hormonal contraception
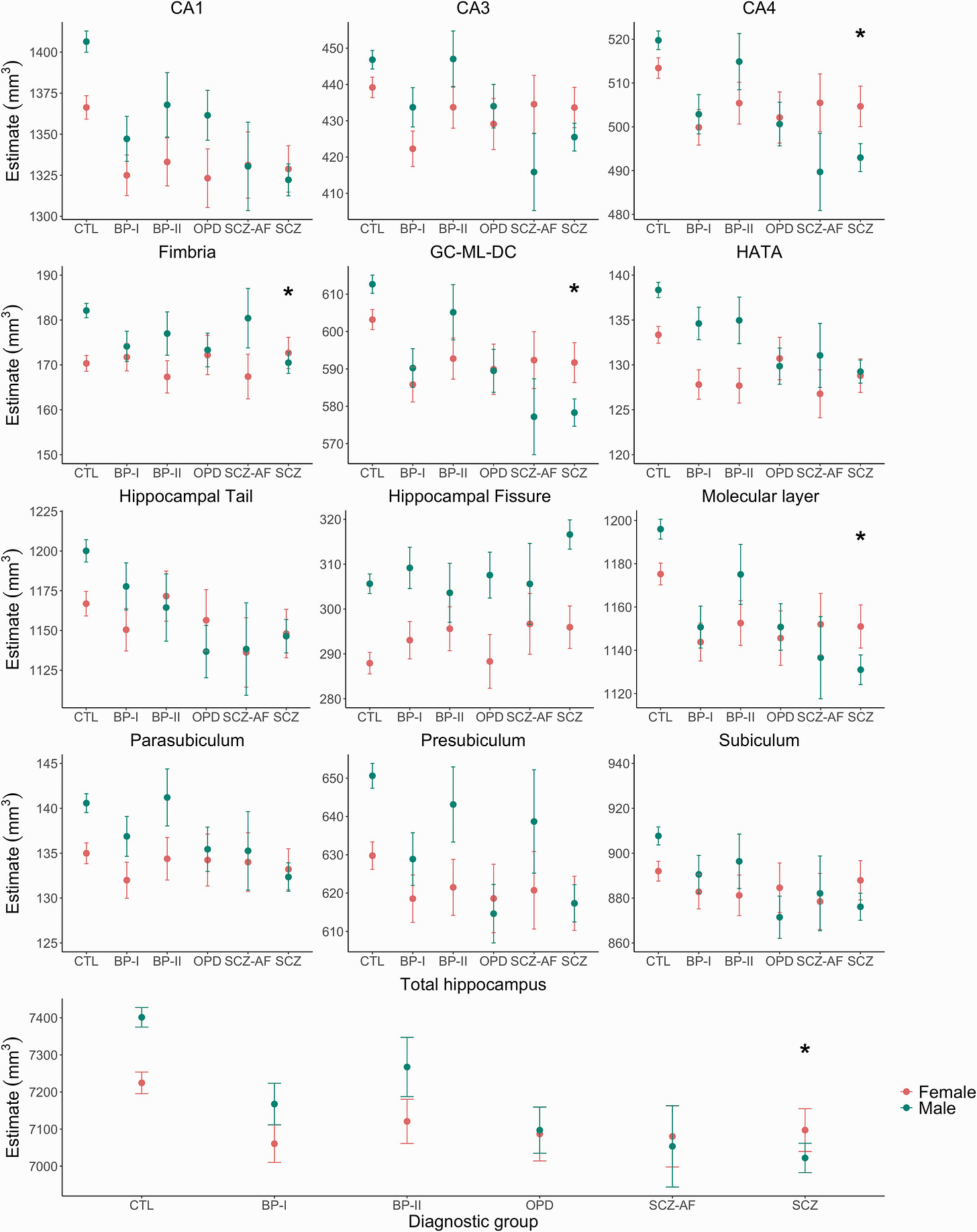
Another well-powered (n=1.5k) neuroimaging study, this time from Norway, investigating the effect of sex and diagnosis (healthy controls, bipolar disorder, schizophrenia) on hippocampal volumes.
In healthy controls, after adjusting for things like total intracranial volume, males had greater hippocampal volumes than females. Perhaps surprisingly, in patients with schizophrenia, it was reversed - males had lower volumes than females. Effect sizes, as expected, were small overall.
Genomic inference of a severe human bottleneck during the Early to Middle Pleistocene transition (via Neurobiology Notes)
Did you hear we almost went extinct between 800,000 - 900,000 years ago? Our numbers dwindled to around 1300 (to put this in perspective, on average, we meet 80,000 other people over the course of a lifetime).
That calculation was made by examining modern genomes, using a form of coalescence to look backward in time - the size of populations thousands of years ago can affect the frequency of alleles in modern day genomes.
Huge props to that small ancestral population for keeping the species going - we all owe you!
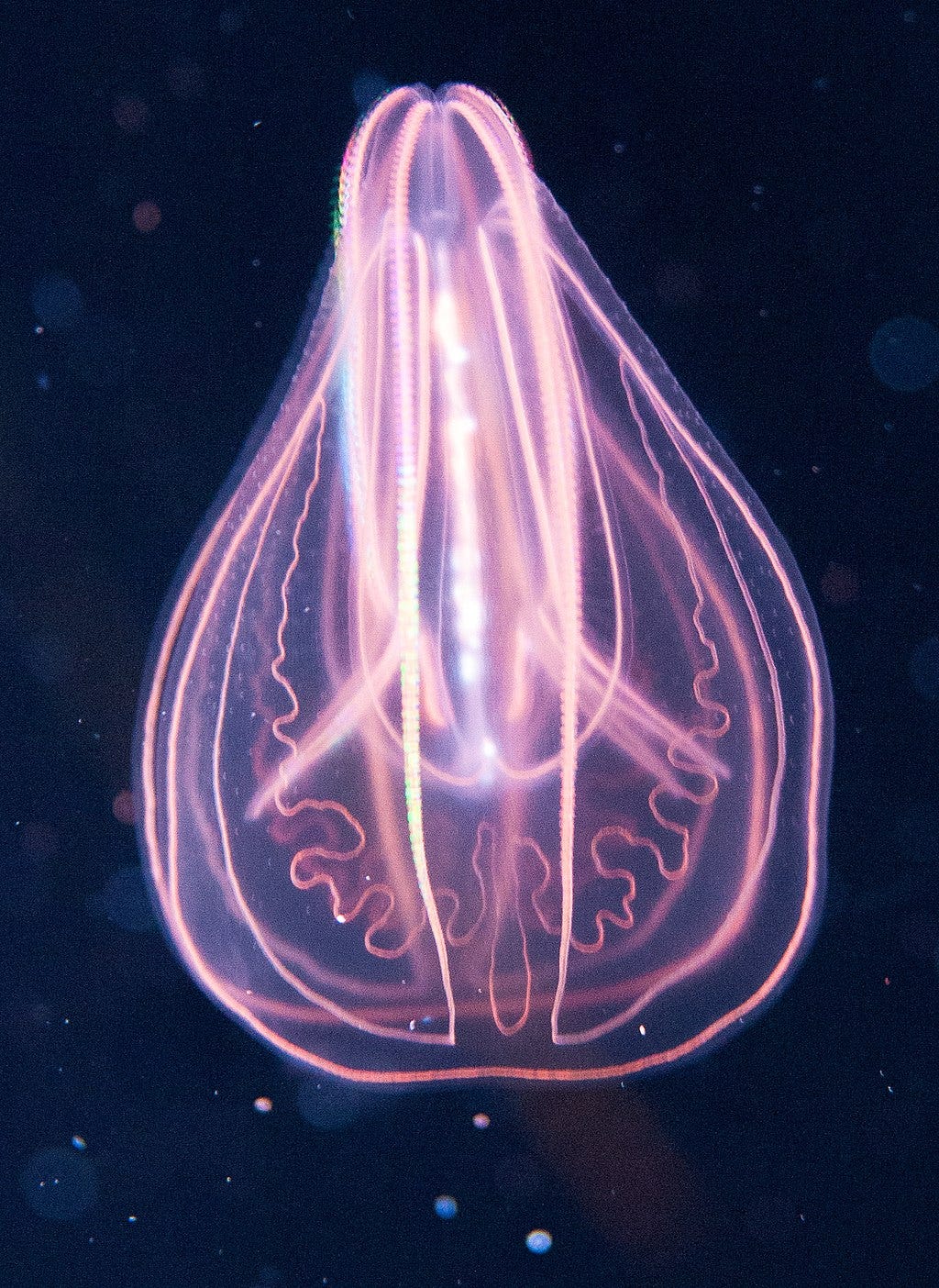
The neuron doctrine states that the brain is composed of discrete, individual cells, that we call neurons. While these may touch, they do not fuse, but instead communicate through junctions, called synapses.
Pawel Burkhardt and colleagues describe a different type of connection in ctenophores (comb jellies). Using electron microscopy they show that its neurones are connected by a continuous membrane rather than synapses. Conforming more to Golgi’s reticular doctrine.
Will aliens have evolved nervous systems more like us, or our ancient relatives, the comb jellies?
Contrary to the popular refrain, opposites do not attract. Instead the rule is assortative mating, whereby a wide range of traits show positive correlation between a couple. This is true for humans, as for many animals.
Horwitz and colleagues undertook a massive analysis of traits within couples - testing 22 traits in a meta-analysis (with sample sizes ranging from the thousands to millions) and 133 in the UK Biobank (79,000 female-male couples).
Politics, religion, educational attainment, and substance use had the highest correlations.
The FTO gene was first linked with obesity in 2007. However, it has been something of a puzzle. The risk variant for obesity in humans seemed to cause weight loss in mice.
I can’t compete with Veera Rajagopal in telling this ‘GWAS story’. But the solution, that the variant promotes brown fat thermogenesis explains why it has different effects in mice at cold compared with ambient temperature, and why it has differing effects in babies compared with adults.
This study described genetic diagnosis for children with unknown developmental disorders referred by regional genetic clinics in the UK and Ireland. Multimodal analysis of genomewide data provided a molecular diagnosis in an impressive 41% of 13k children referred.
Notably, children with African ancestry, those who were extremely premature, or whose mothers had diabetes or took anticonvulsants during pregnancy were less likely to receive a diagnosis.
There is a wide range of analyses for functional brain connectivity - something I’ve found confusing when interpreting research. When a field has so many degrees of researcher freedom, results become less believable.
This paper, suggests that simpler measures of autocorrelation in space (similarity among brain regions close together) and time (similarity at close time-points) can explain more complex descriptions of network topology.
It might be a good way of providing reliable and interpretable measures for resting functional MRI studies.
What happens when you take a cell and strip it down the bare genomic information necessary for survival?
Mycoplasma mycoides cells possessing only essential genes were compared with the ‘non-minimal’ cells from which they were derived. Given enough time, the minimal cell evolved at a faster rate than the non-minimal version and, after 2000 generations, regained its fitness.
Life finds a way.
There are lots of claims that moderate alcohol intake is better than none at all. This is a replicated finding, but is it true? A problem of observational research is confounding. People who are teetotal are different from people who have a moderate alcohol intake in ways unrelated to drinking.
Mendelian Randomisation can be used to disentangle confounding effects - using genetic markers of alcohol consumption gets rid of problems like confounding. This study in a Chinese population shows that no level of drinking is beneficial, alcohol has uniformly negative effects on the cardiovascular system.
To get into the nuts and bolts of Mendelian Randomisation, check out this blog from a bone fide expert, George Davey Smith.
Cheers!
Why do we faint? You can see it as a protective mechanism, making a person lie flat and therefore maintaining blood circulation to the brain. Another side of the heart-brain connection!
Now, the precise mechanisms have been discovered, using optogenetics. Vagal sensory neurones connect the heart to the brain. When activated they trigger hypotension, bradycardia and reduced respiration - this results in loss of consciousness, i.e. fainting.
A challenge of studying oestradiol is the variation within and between individuals. Researchers can have high accuracy by measuring oestradiol in blood but with associated high participant burden and likely low temporal precision (most people aren’t thrilled about daily blood tests).
This paper describes a wearable monitor of oestradiol in sweat. This paper reports good correlation with blood levels but (major warning) in a sample size of two. If it can be replicated at scale, it opens up possibilities for examining how daily fluctuations in oestradiol are associated with other measures of mental or reproductive health.
This is a prime example of how to study the effects of the menstrual cycle on the brain:
Six time-points per participant
Paired with hormone measures
Controlled for water content and blood flow
Significant changes in medial temporal lobe volumes across the cycle, associated with hormone fluctuations.
It was accompanied by a nice commentary from another pioneer in this area, Emily Jacobs.
Everyone thought antipsychotics work through D2 blockade…turns out we might have gone with the wrong receptor.
This elegant study in mice showed antipsychotic efficacy is associated with modulation of D1 receptor neurones. It is a great example of how animal studies can be used in psychosis research. The authors took information from humans (which drugs have best efficacy) and back-translated to find how this efficacy correlated with effects in mice.
A better understanding of how antipsychotics work has big implications for future drug discovery.
Have you ever been in an enclosed space with a distressed, crying baby. It is not pleasant. Part of the reaction seems routed in biology, particularly for mothers.
In mice hearing the sound of crying pups stimulated oxytocin release in the mother whereas other sounds had no effect. (Oxytocin is important for maternal behaviours and lactation.)
Using optogenetics, the precise circuits and neurones triggering this reflex were identified.

Deep brain stimulation isn’t a familiar treatment in the UK - I’m therefore looking across the pond with awe.
Here, surgically implanted devices were used to stimulate the cingulate in patients with treatment resistant depression. The devices also recorded electrical activity of the brain. This activity was able to provide a marker of recovery from depression (though note, n=6 and as it wasn’t a randomised controlled trial we can’t speak about efficacy).
GDF15 is a hormone linked to nausea and weight loss. High levels are associated with certain cancers. GDF15 rises swiftly in pregnancy and remains high throughout. It seems obvious that this hormone causes hyperemesis (nausea and vomiting) in pregnancy. However, not all mothers are susceptible to these effects.
Perhaps counter intuitively, genetic predisposition for high GDF15 protects against hyperemesis in pregnancy. The explanation seems to be that mothers with high baseline levels have been desensitised to its effects. This points to a potential treatment for hyperemesis - gradually up-titrating levels of GDF15 prior to pregnancy (and therefore avoiding the acute, rapid rise).
Read the backstory to this paper from the senior author Stephen O’Rahilly.
Anxiety makes your heart race. But does a racing heart also cause anxiety?
This optogenetics study shows increasing the heart rate of mice produced anxiety-like behaviour, mediated by the posterior insular cortex. This finding lends weight to the James-Lange theory of emotion, that physiological arousal instigates emotional states.
The lead author Karl Deisseroth is one of the developers of optogenetics - I highly recommend his interview on Lex Fridman’s podcast (it amazes when top tier neuroscientists are also working clinically in psychiatry).
You already know how much I like this paper, from last month’s post, Have we been doing neuroimaging wrong?
I don’t think I need to say much more, other than the Nico Dosenbach is a bit of star, having published in Nature for two consecutive years. He also sounds very down to earth. Listen to his own take on this paper. Just a shame he’s a neurologist.
Paper of the year
For anyone prescribing antipsychotics (as well as every patient taking these medications) there comes a time when the question arises; stop or continue? These are powerful medications, not without side-effects, so they should only be taken for good reason. Even the most esteemed schizophrenia researchers such as Robin Murray have highlighted the long-term potential downsides, particularly on brain volume.
Stopping suddenly is not advisable, but what if the dose was reduced gradually over weeks and months? Could this avoid the risk of relapse, while potentially improving other outcomes like social function.
I believe this was a completely valid question to ask, and thanks to this landmark trial we have an answer. Antipsychotic reduction and discontinuation does not improve functioning but does increase the risk of relapse. The findings of this study have clear clinical value. If a patient wishes to stop their meds (I’m sure many will still do) we have a much better understanding of the risks involved.
That’s not why this is my paper of the year, though.
Professor Joanna Moncrieff, the lead author, is a strong advocate that medications like antipsychotics are not beneficial long-term. This has put her at odds with most of mainstream opinion. In science though, we don’t resolve disagreement on social media, by debate, or even through correspondence in journals. We resolve them by experiment. And that is what Professor Moncrieff did. She tested her hypothesis.
The design of this trial gave it every chance of a positive result. Participants were carefully chosen (no-one too risky). Sample size was large (the study had enough power to find non-inferiority within 10%). She collaborated with researchers who didn’t necessarily share her view but would have brought methodological rigour.
Like many big trials, it took time. It of course wasn’t funded by pharma so it took governmental funding. And it took collaboration between researchers, clinicians and patients. It gave us a clear answer - maintenance antipsychotic treatment prevents relapses and is not associated with worse psychosocial outcomes. Professor Moncrieff’s hypothesis was proved wrong but we have all gained new information.
That’s progress. That is science.



I had a blast reading these thank you
Thanks for these excellent links. A quick note: regarding the RADAR trial, throughout you write in a way that suggests broad applicability to the population of antipsychotic consumers. The first sentence in particular explicitly includes "every patient taking these medications". But considering the several on and off-label indications of antipsychotics and the prevalence of use in other disorders (especially over here in the states, see eg https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-020-02895-4/tables/3) it might be good to note, outside of the linked title, that the RADAR trial was conducted on patients with schizophrenia only.